Tran Thi Kim Thanh, Specialist Grade I, Head of the Cardiovascular Department IV at Tâm Đức Heart Hospital, will provide detailed insights in this article.
What is Heart Failure?
Heart failure is a condition in which the heart is unable to pump blood effectively, leading to a deficiency in oxygen and nutrients for the body. While it can occur at any age, heart failure is the leading cause of hospitalization for individuals over 65 years old.
Older patients with heart failure may have chronic cardiovascular diseases, but the condition can also stem from aging or inadequate cardiac monitoring and care.
Elderly patients often have multiple comorbidities, such as hypertension, atrial fibrillation, peripheral vascular disease, coronary artery disease, valvular heart disease, kidney failure, or anemia, resulting in the need for multiple medications.
Symptoms of heart failure in older adults can be subtle. Common signs include progressive shortness of breath during daily activities like bathing, dressing, or putting on shoes; swelling in the legs or abdomen; fatigue; bloating; loss of appetite; nausea; cognitive decline; and persistent coughing.
Causes of Heart Failure
Any of the following conditions can damage or weaken the heart muscle, leading to heart failure:
Coronary Artery Disease
Coronary artery disease is the most common form of heart disease and the leading cause of heart failure. It occurs due to the buildup of fatty deposits in the arteries, leading to atherosclerosis, which reduces blood flow and causes ischemia. A heart attack often occurs suddenly when a coronary artery becomes completely blocked.
Hypertension
When blood pressure is high, the heart must work harder than normal to circulate blood throughout the body. Over time, this increased workload can cause the heart muscle to thicken or weaken, reducing its ability to fill or pump blood effectively.
Valvular Heart Disease
Heart valves ensure that blood flows in the correct direction. Damage to these valves—whether from congenital issues or conditions such as valve stenosis, regurgitation, or infective endocarditis—can obstruct blood flow or allow blood to flow backward. This results in blood accumulation in the heart chambers and lungs, causing the heart to work harder, which can eventually lead to heart failure.
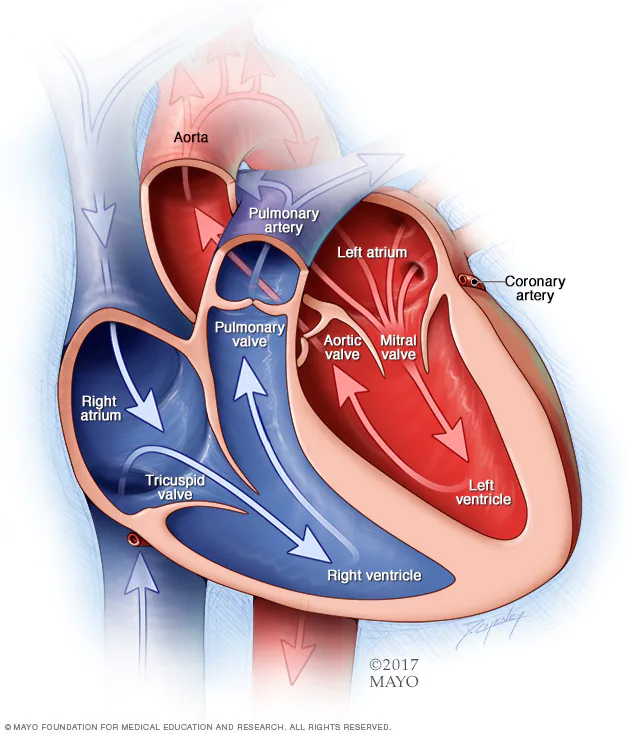
Source: mayoclinic.org
Cardiomyopathy
This condition can arise from various causes, including genetics, infections, alcohol use, and toxic substances like cocaine or chemotherapy agents. Myocarditis, often caused by viruses, including coronaviruses, can lead to left-sided heart failure.
Congenital Heart Disease
This refers to defects in the heart’s chambers and valves that occur during fetal development, creating abnormal blood flow within the heart or between major arteries. These defects require the heart to work harder to pump blood.
Arrhythmias
An irregular heartbeat—whether too fast, too slow, or erratic—places additional strain on the heart to ensure adequate blood delivery to the body’s organs, potentially leading to heart failure.
Other Conditions
Other diseases such as diabetes, HIV, hyperthyroidism, hypothyroidism, and iron overload can also contribute to chronic heart failure.
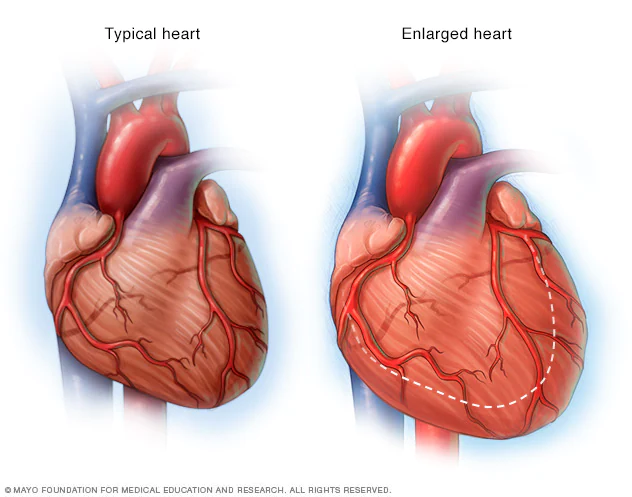
Source: mayoclinic.org
Signs and Symptoms of Heart Failure
Heart failure can be chronic or acute. Symptoms include:
- Shortness of breath during exertion or when lying down
- Fatigue and weakness
- Swelling in the lower legs, ankles, and feet
- Rapid or irregular heartbeat
- Reduced exercise tolerance
- Persistent cough or wheezing with white or pink phlegm
- Abdominal swelling
- Rapid weight gain due to fluid retention
- Nausea and loss of appetite
- Difficulty concentrating or decreased alertness
- Chest pain, especially if heart failure is due to a heart attack
Monitoring Heart Failure Symptoms – When to See a Doctor
You should see a doctor if you experience any of the following signs or symptoms of heart failure:
- Chest pain
- Fainting or severe weakness
- Rapid or irregular heartbeat accompanied by shortness of breath, chest pain, or fainting
- Sudden, severe shortness of breath with pink or white foamy sputum
- If you have been diagnosed with heart failure and notice any sudden worsening of symptoms or new signs, it may indicate that your heart failure is worsening or not responding to treatment.
- Weight gain of 2-3 kg (about 4-6 lbs) or more within a few days.
If you experience any of these symptoms, it is essential to seek medical attention immediately.

How is Heart Failure Treated?
The treatment of heart failure in older adults typically involves a combination of four basic approaches:
- Medications
- Diet
- Monitoring
- Exercise
Medications
Always adhere to the prescribed treatment plan. Take medications on time to avoid missing doses.
Diet
Dietary Guidelines: It is important to limit salt and water intake as advised by your doctor. Generally, heart failure patients should consume less than 2 grams of salt (approximately ½ teaspoon) and less than 1800 ml of water daily.
Specific amounts of salt and water may vary by patient, so consult your doctor for personalized dietary recommendations.
Monitoring
Regularly measure blood pressure, weight, and urine output, and keep a daily log. Patients should bring these records to their follow-up appointments.
Exercise
Appropriate Walking: Exercise is essential for maintaining heart health. Heart failure patients should remain active daily but must be cautious not to overexert themselves. Walking is an effective form of exercise for older adults with heart failure.
Additionally, if patients seek a more tailored exercise program, they should consult their doctor.

Caring for Someone with Heart Failure
If an elderly relative or family member is suffering from heart failure, you can help them in the following ways:
- Ensure they attend regular check-ups as scheduled by their doctor.
- Accompany them to medical appointments.
- Help keep a log of blood pressure, weight, and daily urine output.
- Regularly ask about their condition and observe signs of heart failure, such as shortness of breath, swelling, fatigue, fluid intake, and mental status.
- Monitor symptoms when taking medications and note any changes in their prescriptions during each visit.
- Do not self-medicate with pain relievers, as this could worsen their heart failure.
- Record and report any changes to their doctor.
- While there are many challenges in treating heart failure in older adults, you don’t have to face them alone.
Early treatment and proper care play a crucial role in slowing disease progression, helping patients maintain a better quality of life and peace of mind during treatment.
How to avoid Heart Failure: Healthy Lifestyle Tips and Medical Advice
Preventing heart failure involves managing and controlling conditions that can lead to it, such as coronary artery disease, hypertension, diabetes, and obesity.
You can control or eliminate many risk factors for heart failure by making lifestyle changes and adhering to treatment plans.
Lifestyle changes to help prevent heart failure include:
- Not smoking
- Controlling blood pressure and blood sugar levels
- Maintaining regular physical activity
- Eating healthy foods and reducing salt intake
- Maintaining a healthy weight
- Reducing anxiety and stress
- Undergoing regular cardiovascular check-ups every six months for individuals over 40
- For those with cardiovascular risk factors (obesity, smoking, sedentary lifestyle, alcohol abuse)
- For individuals on immunosuppressive medications
Mostly important, Annual health check-ups for everyone to screen for conditions and risk factors that may lead to heart failure, allowing for timely intervention.



